You may not be demobilized, but you feel disturbing pain sensations while walking, standing or sitting. A sensation like tingling pain from your back through to the buttocks, thighs, feet and toes; then, you might be experiencing sciatica. Any form of pain is bad enough for daily activities. It, however, becomes worse and alter lifestyles when mobility parts like back, legs and feet are directly affected. Pain in mobility parts of the body can stop you from doing all of the things you love, as well as have a bad effect on your mental health.
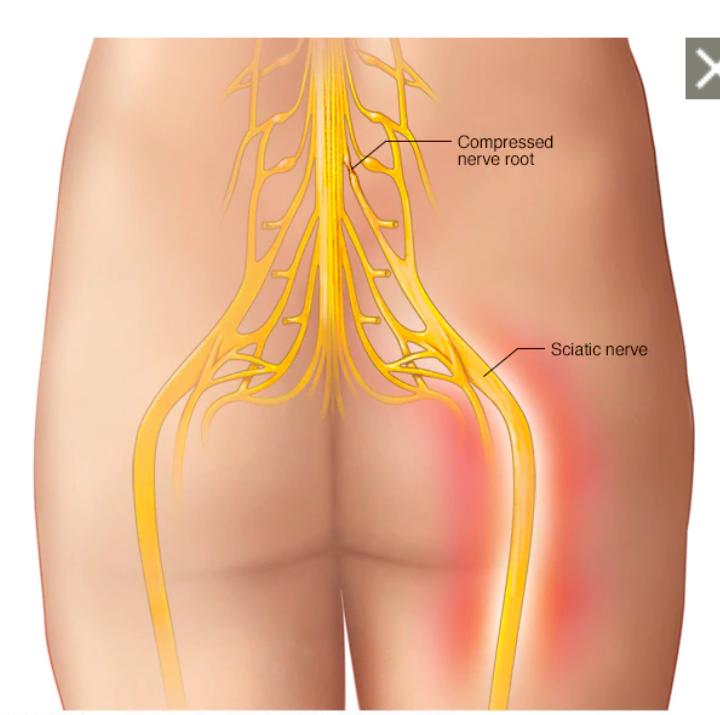
Sciatica is a type of pain that stems from the inflammation of the sciatic nerve. This nerve carries messages from your brain, all the way down your back (spinal cord) to your legs and feet. Normally, one of the signs of sciatica is pain that radiates down one side of your body, starting at the lower back and running down the leg to just below the knee. It can also cause muscle weakness and numbness in the legs.
Usually, sciatica affects only one leg at a time and the symptoms radiate from the lower back or buttock to the thigh and down the leg. Sciatica may cause pain in the front, back, and/or sides of the thigh and leg. But in some rare cases sciatica can affect the two legs at a time particularly if the cause is as a result of degenerative disk.
Symptoms
Sciatica pain may be constant or intermittent. The pain is usually described as a burning sensation or a sharp, shooting pain. The pain is usually more severe in the leg compared to the back. Leg pain commonly occurs more in the calf region below the knee compared to other parts of the leg.
– Altered sensation. Numbness, tingling, and/or a pins-and-needles sensation may be felt at the back of the leg.
–Weakness. Weakness may be felt in the leg and foot. A feeling of heaviness in the affected leg may make it difficult to lift the foot off the floor.
-Change in posture may aggravate or relieve pain. Certain postures may affect sciatica pain: Sciatica pain may feel worse while sitting, trying to stand up, standing for a long time, bending the spine forward, twisting the spine, and/or while coughing.
Pain may increase or remain constant while lying down, causing disturbed sleep. Lying on the back with the knees slightly elevated and propped up with a pillow, or lying on the side with a pillow between the legs, may help relieve the pain in such cases.
The pain may be relieved while walking, applying a heat pack to the rear pelvic area, or doing pelvic exercises. Other symptoms include:
- Lower back pain
- Pain in the rear or leg that is worse when sitting
- Hip pain
- Burning or tingling down the leg
- Weakness, numbness, or a hard time moving the leg or foot
- A constant pain on one side of the rear
- A shooting pain that makes it hard to stand up
Sciatica usually affects only one side of the lower body. Often, the pain extends from the lower back all the way through the back of your thigh and down through your leg. Depending on where the sciatic nerve is affected, the pain may also extend to the foot or toes.
For some people, the pain from sciatica can be severe and disabling. For others, the sciatica pain might be infrequent and irritating, but has the potential to get worse.
Seek medical attention right away if you have:
- Fever and back pain
- Swelling or redness in your back or spine
- Pain that moves down your legs
- Numbness or weakness in the upper thighs, legs, pelvis, or bottom
- Burning when you pee or blood in your pee
- Serious pain
- Loss of bladder or bowel control (leaking or not being able to make it to the toilet in time)
Common causes of sciatica and Risk Factors include:
- Lumbar spinal stenosis (narrowing of the spinal canal in your lower back)
- Degenerative disk disease (breakdown of disks, which act as cushions between the vertebrae)
- Spondylolisthesis (a condition in which one vertebra slips forward over another one)
- Pregnancy
- Muscle spasm in the back or buttocks
Other things that may make you more likely to have sciatica include:
- Aging (which can cause changes in the spine, like bone spurs or herniated disks)
- Diabetes
- Being overweight
- Not exercising regularly
- Wearing high heels
- Sleeping on a mattress that is too hard or too soft
- Smoking
- Your job, especially if it involves driving for long periods of time, twisting your back, or carrying heavy things
Types
Depending on the duration of symptoms and if one or both legs are affected, sciatica can be of different types:
–Acute sciatica. Acute sciatica is a recent onset, 4 to 8-week duration of sciatic nerve pain. The pain may be self-managed and may not typically require medical treatment.
–Chronic sciatica. Chronic sciatica is persistent sciatic nerve pain that lasts for more than 8 weeks and usually does not subside with self-management. Depending on the cause, chronic sciatica may require nonsurgical or surgical treatment.
–Alternating sciatica. Alternating sciatica is sciatic nerve pain that affects both legs alternately. This type of sciatica is rare and may result from degenerative problems in the sacroiliac joint.
–Bilateral sciatica. Bilateral sciatica occurs in both legs together. This type of sciatica is rare and may occur due to degenerative changes in the vertebrae and/or the disc at several spinal levels.
– Wallet sciatica: sciatic pain that occurs while sitting on a wallet (or any object in the back pocket of a trouser).
Diagnosis & Treatment
Although sciatica can be extremely painful, it is very rarely harmful. For most people suffering from sciatica, symptoms generally improve over a few weeks with conservative treatment. There are other options such as spinal injections, which can give immediate relief to very bad pain.
If your doctor thinks you have sciatica, you’ll get a physical examination so they can check your reflexes and see how strong your muscles are. They might have you do certain activities, like walking on your heels or toes, to see what’s causing your pain.
If your pain is severe, the doctor might order imaging tests like X-Ray, CT scan, MRI EMG etc. to check for bone spurs and herniated disks. You could get tests like:
Most people with sciatica feel better after self-care activities or at-home remedies like:
- Using cold or hot packs
- Stretching
- Over-the-counter pain medication
But if your pain isn’t getting better, your doctor might suggest other options.
Medication: Anti-inflammatories, anti-seizures, muscle relaxants, narcotics and anti-depressants. See your doctor for the best medication for you.
A physical therapist can show you how to do exercises that will improve your posture and make you more flexible. They’ll also make the muscles that support your back stronger.
Steroid injections
Your doctor might recommend you get steroid injections shot. They’ll give you a shot that has medicine to help with inflammation around the nerve, which can help reduce your pain. The effects usually last a few months, but they’ll wear off over time.
Surgery
If you have extreme pain that doesn’t get better, weakness, or a loss of bladder or bowel control, your doctor might recommend surgery. They’ll take out the bone spur or herniated disk that’s pressing on your nerves and causing your pain.
Prevention
Sciatica once it started comes and go, so it may not be easy to completely prevent it. We can reduce sciatica problems if we consciously protect our back via:
-Regular exercise. To keep back and core muscle for posture and alignment strong
-Maintain proper posture when you sit. Use seat with good lower back support, armrests and a swivel base. You can place a pillow or rolled towel in the small of the back to maintain normal curve. Keep your kneels and hips level
-Use good body mechanics. if you stand for long periods, rest one foot on a stool or small box from time to time. When you lift something heavy, let your lower extremities do the work. Move straight up and down. Keep your back straight and bend only at the knees. Avoid lifting and twisting simultaneously.